What Is Infectious Gastroenteritis? Understanding the Stomach Bug
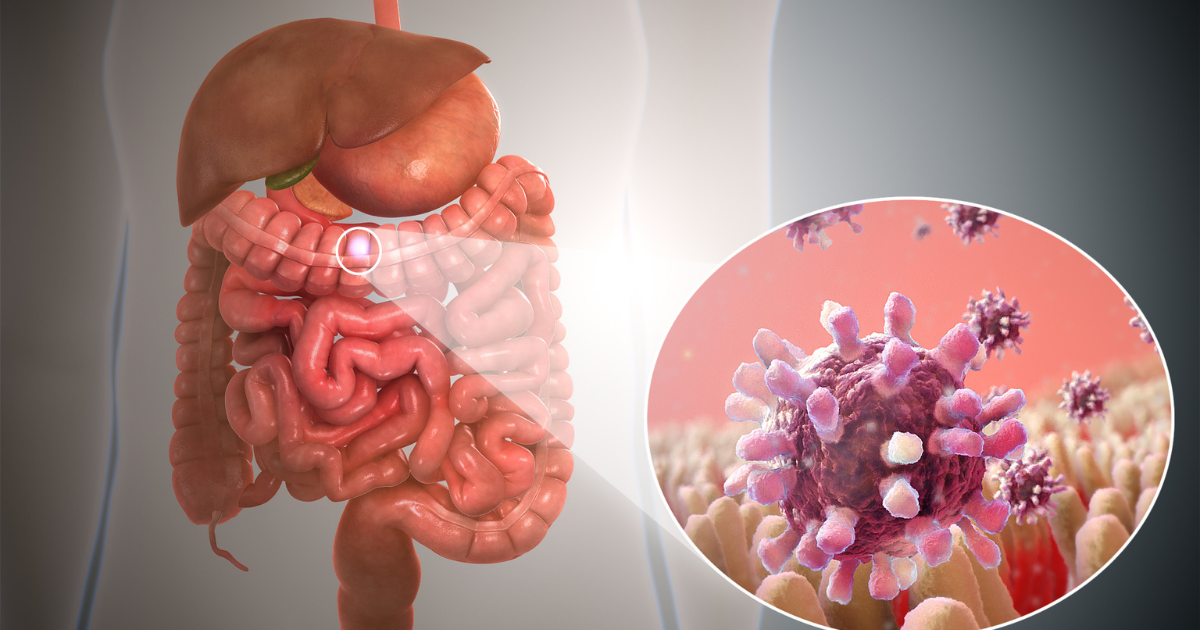
Infectious gastroenteritis, often called the stomach flu, is an inflammation of the stomach and intestines caused by a viral, bacterial, or parasitic infection, leading to unpleasant symptoms like diarrhea, vomiting, and abdominal cramps.
Introduction: Beyond the Stomach Flu
What is infectious gastroenteritis? It’s a common ailment, often dismissed as a simple “stomach bug,” but it’s more than just a passing inconvenience. Understanding its causes, symptoms, and prevention strategies is crucial for maintaining good health, especially in vulnerable populations like children and the elderly. This article provides a comprehensive overview of what infectious gastroenteritis entails, equipping you with the knowledge to recognize, manage, and prevent this troublesome condition.
Causes of Infectious Gastroenteritis
Several pathogens can trigger infectious gastroenteritis, broadly categorized into viruses, bacteria, and parasites. Understanding the specific causes helps in determining the appropriate treatment and prevention strategies.
- Viruses: The most frequent culprits are norovirus and rotavirus. Norovirus is highly contagious and often responsible for outbreaks, particularly in crowded settings like schools and cruise ships. Rotavirus is a leading cause of gastroenteritis in infants and young children, although vaccination has significantly reduced its prevalence. Other viral causes include adenovirus and astrovirus.
- Bacteria: Common bacterial causes include Salmonella, E. coli (especially E. coli O157:H7), Campylobacter, and Shigella. Bacterial infections are often associated with contaminated food or water.
- Parasites: Parasitic infections like Giardia lamblia and Cryptosporidium can also cause gastroenteritis. These parasites are often found in contaminated water sources.
Symptoms of Infectious Gastroenteritis
The symptoms of infectious gastroenteritis can vary in severity depending on the causative agent and the individual’s health status. Common symptoms include:
- Diarrhea: Frequent, watery stools are a hallmark symptom.
- Vomiting: Can occur suddenly and be quite severe.
- Abdominal cramps and pain: Often experienced before or during bowel movements.
- Nausea: A feeling of unease and the urge to vomit.
- Fever: May be present, especially in bacterial infections.
- Headache: Can accompany other symptoms.
- Muscle aches: A general feeling of malaise and body aches.
Transmission and Risk Factors
Understanding how infectious gastroenteritis spreads is essential for prevention. It is highly contagious and typically transmitted through:
- Fecal-oral route: This is the most common mode of transmission, occurring when contaminated feces enter the mouth. This can happen through:
- Consuming contaminated food or water.
- Touching contaminated surfaces and then touching your mouth.
- Close contact with an infected person.
- Person-to-person contact: Especially common in settings like daycare centers and nursing homes.
- Contaminated surfaces: Viruses and bacteria can survive on surfaces for extended periods.
Certain factors increase the risk of developing infectious gastroenteritis:
- Young children: Their immune systems are still developing, and they are more likely to put things in their mouths.
- Elderly individuals: Their immune systems may be weakened, and they may have underlying health conditions.
- Individuals with weakened immune systems: Such as those undergoing chemotherapy or with HIV/AIDS.
- Travelers: Exposure to unfamiliar pathogens in different regions can increase the risk.
- Those who consume contaminated food or water.
Diagnosis and Treatment
Diagnosis of infectious gastroenteritis typically relies on the patient’s symptoms and medical history. In severe cases, a stool sample may be collected to identify the specific causative agent.
Treatment primarily focuses on relieving symptoms and preventing dehydration. Key strategies include:
- Oral rehydration: Drinking plenty of fluids, such as water, electrolyte solutions (pedialyte), or clear broths, to replace lost fluids and electrolytes.
- Rest: Allowing the body to recover.
- Diet: Starting with small, bland meals, such as toast, crackers, and bananas (the BRAT diet). Avoid dairy products, fatty foods, and sugary drinks.
- Medications: Anti-diarrheal medications may be used in some cases, but it’s crucial to consult with a healthcare professional before taking any medication, especially for children. Antibiotics are typically not effective for viral gastroenteritis and should only be used if a bacterial infection is confirmed. Anti-emetics can help reduce nausea and vomiting, but should also be taken under medical supervision.
Prevention Strategies
Preventing infectious gastroenteritis requires a multi-pronged approach focused on hygiene and food safety.
- Handwashing: Frequent and thorough handwashing with soap and water, especially after using the toilet, before eating, and after handling food.
- Safe food handling: Properly cooking and storing food to prevent bacterial growth. Avoid cross-contamination by using separate cutting boards for raw meats and vegetables.
- Safe water consumption: Drinking clean, treated water. When traveling to areas with questionable water quality, use bottled water or boil water before drinking.
- Vaccination: Rotavirus vaccine is highly effective in preventing rotavirus gastroenteritis in infants.
- Surface disinfection: Regularly disinfecting frequently touched surfaces, such as doorknobs, light switches, and countertops, especially during outbreaks.
- Avoid sharing personal items: Sharing utensils, cups, and towels can facilitate the spread of infection.
Complications of Infectious Gastroenteritis
While most cases of infectious gastroenteritis resolve on their own within a few days, complications can occur, particularly in vulnerable populations.
- Dehydration: The most common complication, especially in young children and the elderly. Signs of dehydration include decreased urination, dry mouth, dizziness, and weakness. Severe dehydration can be life-threatening.
- Electrolyte imbalance: Diarrhea and vomiting can lead to loss of essential electrolytes, such as sodium, potassium, and chloride. Electrolyte imbalances can cause muscle cramps, irregular heartbeats, and seizures.
- Kidney failure: Severe dehydration can strain the kidneys and lead to kidney failure.
- Post-infectious irritable bowel syndrome (PI-IBS): In some cases, gastroenteritis can trigger long-term digestive problems, such as IBS.
What to Do If You Suspect Infectious Gastroenteritis
If you suspect you have infectious gastroenteritis, it’s crucial to take steps to prevent its spread and manage your symptoms.
- Stay home: Avoid going to work or school to prevent infecting others.
- Hydrate: Drink plenty of fluids to replace lost fluids and electrolytes.
- Rest: Allow your body to recover.
- Practice good hygiene: Wash your hands frequently and disinfect surfaces.
- Consult a doctor: Seek medical attention if you experience severe symptoms, such as high fever, bloody stools, severe dehydration, or persistent vomiting.
Frequently Asked Questions
What is the difference between infectious gastroenteritis and food poisoning?
While both can cause similar symptoms, infectious gastroenteritis is typically caused by viruses, bacteria, or parasites that infect the digestive system, while food poisoning results from consuming food contaminated with toxins produced by bacteria, such as Staphylococcus aureus or Bacillus cereus. The onset of symptoms can sometimes help distinguish between the two, with food poisoning often having a more rapid onset.
How long is infectious gastroenteritis contagious?
The duration of contagiousness varies depending on the causative agent. Norovirus, for example, is highly contagious and can be spread even after symptoms have resolved, sometimes for up to two weeks. Generally, it is best to consider yourself contagious as long as you are experiencing symptoms and for at least a few days afterwards.
When should I see a doctor for infectious gastroenteritis?
You should seek medical attention if you experience signs of severe dehydration, such as decreased urination, dizziness, or weakness; bloody stools; high fever (over 101°F or 38.3°C); persistent vomiting; or severe abdominal pain. Infants, young children, and the elderly are at higher risk of complications and should be monitored closely.
Can I prevent infectious gastroenteritis with probiotics?
While some studies suggest that probiotics may help reduce the duration and severity of gastroenteritis, particularly rotavirus-induced gastroenteritis in children, the evidence is not conclusive. Probiotics may help restore the balance of gut bacteria after an infection, but they are not a guaranteed preventive measure.
Are antibiotics effective against infectious gastroenteritis?
Antibiotics are not effective against viral gastroenteritis, which is the most common type. They are only useful if a bacterial infection is confirmed by a stool test. Overuse of antibiotics can contribute to antibiotic resistance.
Can I catch infectious gastroenteritis from contaminated surfaces?
Yes, viruses and bacteria can survive on surfaces for varying lengths of time. Norovirus, for example, can persist on surfaces for days. Frequent cleaning and disinfection of frequently touched surfaces, especially in bathrooms and kitchens, can help prevent the spread of infection.
What is the best way to rehydrate during infectious gastroenteritis?
Oral rehydration solutions (ORS), such as Pedialyte or Ceralyte, are ideal for rehydration because they contain the right balance of electrolytes to replace those lost through diarrhea and vomiting. Water is also important, but ORS help restore electrolyte balance more effectively.
Is it safe to eat dairy products during infectious gastroenteritis?
Many people experience temporary lactose intolerance after gastroenteritis because the infection can damage the lining of the small intestine, which produces lactase (the enzyme that digests lactose). It’s generally best to avoid dairy products until your symptoms have resolved.
Can I get infectious gastroenteritis from swimming pools?
Yes, Cryptosporidium and other pathogens can contaminate swimming pools, especially if they are not properly chlorinated. Swallowing contaminated water can lead to infection. Avoid swallowing pool water and shower before entering the pool.
Is there a vaccine for infectious gastroenteritis?
Yes, there are vaccines for rotavirus, which is a leading cause of gastroenteritis in infants and young children. The rotavirus vaccine is typically administered in a series of doses during infancy.
How can I protect my family from infectious gastroenteritis during an outbreak?
During an outbreak, emphasize frequent handwashing, especially after using the toilet, before eating, and after touching potentially contaminated surfaces. Isolate infected individuals, disinfect surfaces regularly, and avoid sharing personal items.
Can infectious gastroenteritis cause long-term health problems?
In most cases, infectious gastroenteritis is a self-limiting illness that resolves without long-term consequences. However, in some individuals, it can trigger post-infectious irritable bowel syndrome (PI-IBS), leading to chronic digestive symptoms. Severe dehydration can also lead to kidney damage if left untreated.